Negative Dysphotopsia-Causes & Symptom
- Subhabrata Bhattacharya
- Oct 13, 2018
- 6 min read
Updated: Jan 19
In recent times the topic of Negative Dysphotopsia or dark temporal shadow after cataract surgery has gained some interest among surgeons, ever since the phenomenon was first discussed by James Davison in his article published in JCRS in 2000. Davison’s paper first drew the attention of the medical fraternity to the potential visual disturbance that may be caused in some patients post cataract surgery.
Samuel Masket, in his paper published in JCRS in 2011 describes Negative Dysphotopsia (ND) as a dark crescent in temporal field of vision. Note, this condition is different from positive dysphotopsia, wherein patients suffer from undesired optical halos and other photic issues.
Since the work of Davison and Masket, different clinical researchers and at different points of time have brought out varying causes of ND. However, the following has often been pointed out as a cause of it –
a. ND may be associated with many different types of Posterior Chamber in the bag fixated IOLs, regardless of material/RI/round or squared edge.
b. Symptoms of ND have been reported to have been reduced by pharmacologic pupil dilation and increased by pupil constriction in the paper published by Masket in 2011.
c. It is not related to pre operative or post operative ametropia
d. ND symptoms have been reported typically within 1 month of cataract surgery with PC IOLs, but in most cases subside over a period. Very few cases of severe and persistent symptoms have been reported.
In their paper, Negative dysphotopsia: The enigmatic penumbra, Jack T. Holladay, MD, MSEE, Huawei Zhao, PhD, Carina R. Reisin, PhD, J CATARACT REFRACT SURG - VOL 38, JULY 201, the authors presented dysphotopsia in terms of Type 1, Type 2 and Type 3. They point out that unwanted shadows in most optical systems are a result of discontinuities in the system where two adjacent incident rays follow entirely two different paths.
Type 1:
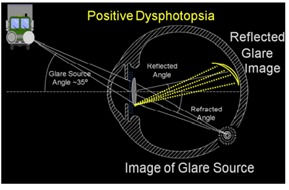
The rays that form the positive dysphotopsia on the tempo[1]ral retina (reflected glare image) from the square or truncated edge optic would be absent from the refracted image of the light source (image of glare source). The missing rays would cause a variation in the intensity of the image, which would be described as abnormal
In their study, Negative dysphotopsia: The enigmatic penumbra, Holladay et al describes that a glare source located approximately 35 deg off the visual axis creates an internal reflection within the IOL that is projected on to the temporal retina. They point out that for acrylic lens with refractive index of 1.55, this critical angle for total angle of reflection is around 59.5 degrees. Such total internal reflections are of brighter intensity with IOL than that of the natural crystalline lens. The internally reflected rays cause positive dysphotopsia on the temporal retina while causing partial shadows on the nasal retina. Such shadows however will only be visible when the pupil is large. Under normal photopic or high mesopic conditions, the pupil is generally too small to allow a ray from 35 degrees to strike the nasal edge of the IOL and cause a shadow.
Key points - Type 1
· Disappears with pupil constriction
· Occurs from light at a source near 35 degrees from visual field
· Type 1 shadow is not what is typically described as negative dysphotopsia
· Can be described as scotoma or steaky vision rather than absolute scotoma
Type 2:
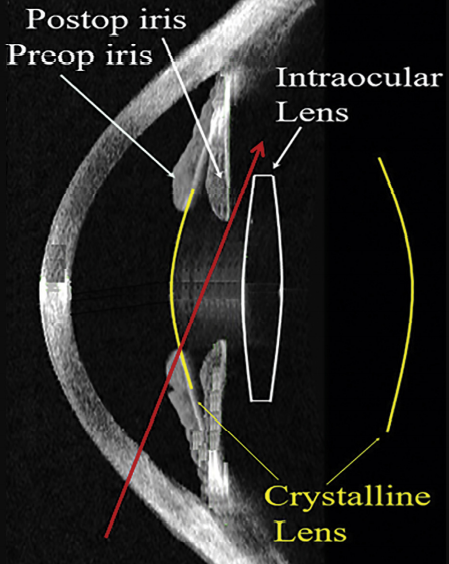
The above image shows the anatomical features preoperative and postoperative. After removal of the larger and thicker crystalline lens, the iris shifts posteriorly (mean 0.8 mm), but a gap is created between the posterior iris and anterior IOL (mean 0.45 mm).6,15 In
the crystalline lens, all rays entering the pupil will pass through the lens. In a capsular bag–fixated IOL, peripheral light rays can access this gap and the unrefracted rays can miss the IOL completely explains Jay C. Erie, MD, Michael J. Simpson, PhD, Mark H. Bandhauer, MS, in their publication A modified intraocular lens design to reduce negative dysphotopsia
The red ray just misses the IOL and is not refracted, while the blue ray is refracted by the anterior surface and then the posterior surface of the IOL. The dark region would appear as a shadow if it fell on functional retina (type 2 shadow)
Image source: J Cataract Refract Surg 2012; 38:1251–1265
Type 2 dysphotopsia is caused by one ray of light entering the pupil that misses the IOL and goes un refracted before reaching the peripheral retina, while another ray of light is refracted by the edge of the IOL or the posterior surface of the IOL. Thus Holladay notes that all IOL which are positive powered and converges rays of light create such shadow as some light is converged and some light misses the IOL and passes through the gap between the IOL and the pupil. The shadow is formed by the angle formed between two light rays - one refracted and the other unrefracted or undeviated.
Holladay notes that Type 2 dysphotopsia:
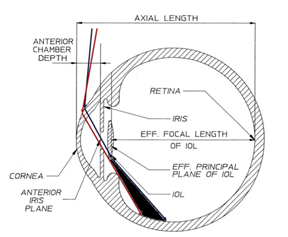
· Occurs only when the IOL is seated deep inside, that is there is significant gap between the IOL and the pupil.
· In their experiment, Holladay notes that the IOL should be sitting at least 2.3mm behind the iris.
Type 3:
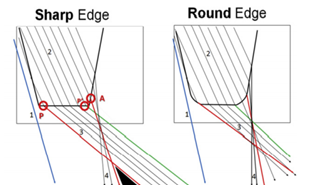
Ray tracing of sharp-edged and round-edged optics. A sharp or truncated edge will have sharp corners anteriorly and pos[1]teriorly versus the partially rounded edge corners. (See Figure 2 for radii details.) On the posterior corner of the sharp edge, rays that pass through the edge (3) are refracted more posteriorly than rays passing through the posterior surface (4). For the sharp edge, a shadow (type 3) is present between red rays 3 and 4. The red ray 3 passing through point “P” determines the posterior boundary and the red ray 4 passing through point “A” determines the anterior boundary of the type 3 shadow
Type 3 dysphotopsia happens when there is a region of shadow created by the rays refracted by the sharp truncated edge of the IOL and the rays refracted by the posterior surface of the IOL that pass near the edges. The deviation in refracted ray of light between the two rays create a shadow. In the figure above, the rays from the sharp edge of the square edge IOL passing through point P is refracted posteriorly, while rays passing through the point A are refracted anterior thus creating a shadow bounded by the two rays of light from point P and point A.
Type 3 dysphotopsia - Key points
· Small pupil increases negative dysphotopsia perception.
· Increased distance between the pupil and IOL with a high refractive index.
· Square edge IOLs have more incidence than rounded shaped IOLs
· More frequently observed with acrylic IOLs than silicone IOLs
Some Key points overall for negative dysphotopsia:
a. Holladay notes that patients with higher angle kappa are at more risk for negative dysphotopsia. Note patients with hyperopia are noted to have higher angle kappa.
b. Very high dioptric power of the IOL (Hyperopic Eyes).
c. Smaller photopic pupil were seen to have more ND in Holladay’s ray tracing study (in contradiction to Masker study)
However, both Masket and Holladay have found out that the incidence of Negative Dysphotopsia is less, when the optic-haptic junction is placed horizontally. Hence it is strongly advised (in cases of non-TORIC ), surgeons who find frequent complaint of patients, may place the IOL oriented horizontally, aligning the haptics on the 0/180 deg meridian.
In a very rare case of persistent complaint of patient with ND, despite horizontal placement of IOL in the bag, the following has been advised in Masket and Holladay papers for surgical intervention :
a. Removal of anterior rim of capsulorhexis from the nasal part is the safest and first step to try to reduce persistent complaints of ND.
b. IOL lens exchange in the sulcus as a last step to mitigate patient condition.
c. Reverse optic capture
Update:
Dr S Navneeth Kumar, a renowned surgeon from Arvind Eye Care has kindly made a video of the article. This video is now available in the below link:
-------------------------------------------------
Source :
1. James Davison : Positive and Negative Dysphotopsia in acrylic IOL ; JCRS 2000
2. Jack Holladay : Negative Dysphotopsia : Causes and rationale for treatment ; JCRS 2017
3. Samuel Masket : Pseudophakic Negative Dysphotopsia ; JCRS 2011
4. Negative dysphotopsia: The enigmatic penumbra, Jack T. Holladay, MD, MSEE, Huawei Zhao, PhD, Carina R. Reisin, PhD
5. A modified intraocular lens design to reduce negative dysphotopsia Jay C. Erie, MD, Michael J. Simpson, PhD, Mark H. Bandhauer, MS; JCRS 2019.


